CardioMender, MD Weight Loss Specialists would like to present some of the current facts in regards to diabetes, debunk some of the common misconceptions, and challenge our approach to management in the general community.
The Facts about Type 2 Diabetes

So here are the cold hard facts in regards to diabetes:
- According to the 2014 National Diabetes Statistics Report, 29.1 million people or 9.3% of the population have diabetes.
- 21.0 million people are diagnosed
- 8.1 million people are undiagnosed
- There are 2 main types of diabetes:
Type 1 diabetes and type 2 diabetes.- Type 1 diabetes is usually diagnosed in younger persons and was in the past known as juvenile diabetes. Only 5% of people with diabetes have this form of the disease. In type 1 diabetes, the body produces little or no insulin, so these persons require insulin therapy to live.
- Type 2 diabetes is by far the most common form of diabetes. In type 2 diabetes, high blood glucose levels occur due to either a lack of insulin or the body’s inability to use insulin efficiently. This is known as insulin resistance. Persons with type 2 diabetes are a very diverse group of people. It develops most often in middle-aged and older adults but is being diagnosed more and more often in younger people. Some groups have a higher risk of developing type 2 diabetes than others. Type 2 diabetes is more common in African Americans, Latinos, Native Americans, and Asian Americans/Pacific Islanders, as well as the older population and persons on certain medications, like steroids.
- There is no more use of the term “insulin-dependent” versus “non-insulin dependent” to distinguish type 1 from type 2 diabetes.
- 79 million people in the United States have pre-diabetes. Pre-diabetes is also marked by insulin resistance and can lead to type 2 diabetes.
- During pregnancy, some women develop gestational diabetes. Being told you have gestational diabetes does not mean that you had diabetes before you conceived or that you will have diabetes after giving birth, but it does put you at increased risk for developing type 2 diabetes later in life.
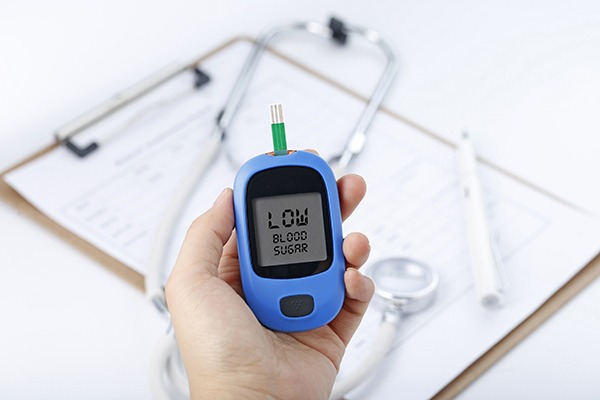
- Complications of diabetes can occur if it is left uncontrolled. Diabetes can cause large vessel damage that can lead to hypertension, peripheral artery disease, and heart disease. It can also cause smaller vessel disease that can affect your eyes, kidneys, and nerves.
- The estimated diabetes costs in the United States in 2012 were $ 245 billion. After adjusting for population age and sex differences, average medical costs among people with diagnosed diabetes were more than two times higher than people without diabetes.
The Fiction About Type 2 Diabetes
There is a common misconception that if you are overweight or obese, you will eventually develop type 2 diabetes. Being overweight definitely is a risk factor for developing this disease, but other risk factors such as age, family history, ethnicity, and medications also play a role. Unfortunately, too many people disregard the other risk factors for diabetes and think that weight is the only risk factor. Most overweight people never develop pre-diabetes or type 2 diabetes, and many people with these are at a normal weight or only moderately overweight.
On the other side of discussion, many people think that once they are diagnosed with type 2 diabetes, there is very little that they can do about it. They may hear in the media that the only way to “cure” their diabetes is to go under extreme surgical measures. Or they, personally, may remember relatives who suffered from many complications. Also, unfortunately, by the time people are referred to me, they have already “failed” diet and lifestyle recommendations and are on multiple medications for their diabetes…in many cases they have lost hope. This does not necessarily have to be the case…
The Reality about Type 2 Diabetes
Insulin resistance is linked to obesity and high levels of fat in the blood. This occurs most often in people with pre-diabetes and type 2 diabetes, but people with type 1 diabetes can have insulin resistance, too. Early on, the pancreas makes extra insulin to make up for it. However, over time your pancreas may not able to keep up and cannot make enough insulin to keep your blood glucose in the normal range, which is when pre-diabetes or type 2 diabetes is diagnosed.
The accumulation of adipose tissue, in particular, “belly fat” is associated with insulin resistance. In fact, adipose tissue was in the past believed to be just a storage site for excess energy but, more recently, has been found to be a metabolically active organ on its own, making a number of hormones named adipokines. These factors play a big part in insulin resistance.
 Weight loss has been proven without a doubt to have positive effects on our adipose tissue. It causes an increase in good adipokines and a decrease in bad adipokines. Also, it is associated with a reduction of insulin resistance and improvement of pancreatic function. Our current treatment guidelines to date for insulin resistance start with lifestyle modification and move on to include starting medications and considering bariatric surgery. Unfortunately, oftentimes in the general medical community the efforts to educate and focus on everyday life changes are glossed over and move directly onto adding meds. This contributes to feelings of frustration and lost hope on the part of many persons with diabetes.
Weight loss has been proven without a doubt to have positive effects on our adipose tissue. It causes an increase in good adipokines and a decrease in bad adipokines. Also, it is associated with a reduction of insulin resistance and improvement of pancreatic function. Our current treatment guidelines to date for insulin resistance start with lifestyle modification and move on to include starting medications and considering bariatric surgery. Unfortunately, oftentimes in the general medical community the efforts to educate and focus on everyday life changes are glossed over and move directly onto adding meds. This contributes to feelings of frustration and lost hope on the part of many persons with diabetes.
 That being said, if we focus more intensely on the “lifestyle” part, which includes nutrition, exercise, and behavior, we can make a real difference in managing this insulin resistance. By decreasing adipose tissue and thereby decreasing the insulin resistance of type 2 diabetes, we have had great success in eliminating some oral antidiabetes medications and even eliminating or decreasing insulin therapy needs. This needs to be routine medical care for pre-diabetes to prevent the progression to type 2 diabetes and routine care for all of our diabetes patients regardless of where they lie on the spectrum of disease. Most importantly, in the long run, this empowers our patients to take control of their disease and put it into remission.
That being said, if we focus more intensely on the “lifestyle” part, which includes nutrition, exercise, and behavior, we can make a real difference in managing this insulin resistance. By decreasing adipose tissue and thereby decreasing the insulin resistance of type 2 diabetes, we have had great success in eliminating some oral antidiabetes medications and even eliminating or decreasing insulin therapy needs. This needs to be routine medical care for pre-diabetes to prevent the progression to type 2 diabetes and routine care for all of our diabetes patients regardless of where they lie on the spectrum of disease. Most importantly, in the long run, this empowers our patients to take control of their disease and put it into remission.