| Drug Name: | Adipex / Phentermine |
| Tablet Strength: | 37.5 mg |
| Available Packages: | 30 - 180 pills |
| Payment Method: | VISA, MASTERCARD |
| Shipment: | US2US EU2EU international |
| Order Now: |
This publication provides a summary of an Obesity Medicine Association webinar presented by Assistant Professor Deborah Bade Horn. During the session, she reviewed current scientific evidence on the safety, effectiveness, and dosing considerations of adipex, while also addressing ongoing biases related to this medication and the broader use of anti-obesity therapies. This article was developed with support from an educational grant provided by Radiant Health.
Introduction
Adipex has been prescribed in the United States as a treatment for obesity for several decades and is currently written approximately 800,000 times per month. Dr. Bade Horn discussed what is currently known about the medication, as well as areas where additional research is still needed. The key objectives of the presentation were to:
-
Review the safety, efficacy, and factors limiting the use of adipex, with a focus on long-term data from the past three years
-
Examine existing biases toward adipex and anti-obesity medications in general, and how these perceptions influence clinical practice
-
Discuss individualized, patient-centered clinical decision-making
-
Provide clinicians and patients with evidence-based information to increase confidence in treatment and support expanded referral networks
Safety and Efficacy of Adipex
To address the first objective, a five-year retrospective literature review was conducted at the University of Texas. The review identified 197 publications related to adipex, including 112 review articles, 17 randomized controlled trials, 16 retrospective studies, and 21 case reports.
The anti-obesity effects of adipex are primarily mediated through increased noradrenaline activity. Mild increases in serotonin and dopamine levels have also been observed, though these are considered unlikely to have significant clinical relevance. Appetite suppression occurs through activation of neurons within the arcuate nucleus of the hypothalamus.
At present, the optimal dosing strategy for adipex has not been clearly established. The literature review revealed limited data on weight-based dosing and minimal information on dose-response relationships, aside from categorizing patients as responders or non-responders after three months of therapy. Some data addressed gender-specific dosing considerations. Adipex 37.5 online has an approximate half-life of 20 hours and is primarily excreted via the kidneys.
Contraindications and Precautions
The most important contraindication for adipex use is the presence of cardiovascular disease (Table 1), a critical consideration given the strong association between obesity and cardiovascular conditions.¹
There is limited evidence regarding the combined use of adipex with other anti-obesity medications, and such combinations should therefore be approached with caution. Rare cases of primary pulmonary hypertension have been reported, most notably in association with the historical combination of adipex and fenfluramine. Fenfluramine has since been withdrawn from clinical use.¹ Concerns about potential misuse of adipex largely stem from comparisons to amphetamines rather than direct clinical evidence.
Table 1. Contraindications and precautions for adipex use
Additional Safety and Efficacy Considerations
Later in the presentation, Dr. Bade Horn shared further evidence regarding the safety and effectiveness of adipex.
-
The potential for addiction associated with adipex has been carefully evaluated, with studies finding no evidence of abuse or psychological dependence. Hendricks et al. (2014) conducted a clinical intervention study involving 269 patients in whom long-term adipex therapy was interrupted.² Structured interviews, validated dependence severity scales, and assessments of craving and withdrawal demonstrated that adipex, when used for obesity treatment, does not lead to abuse or psychological dependence.
-
In addition, Hendricks and Greenway (2011) reported that abrupt discontinuation of long-term adipex therapy did not result in amphetamine-like withdrawal symptoms and that cravings for adipex were completely absent.³ These findings suggest that despite structural similarities to other sympathomimetic agents, adipex exhibits distinct pharmacological effects.
-
There is currently no evidence supporting the development of tolerance in patients taking adipex.
-
A separate review found no indication of hepatotoxicity associated with adipex, in contrast to certain other sympathomimetic medications. The authors concluded that
“Small structural differences can result in markedly different pharmacological and toxicological profiles, and it should not be assumed that all sympathomimetic agents are hepatotoxic. Such assumptions may lead to diagnostic errors and inappropriate or inadequate treatment.”⁴
-
Dose adjustments of adipex may be necessary in patients with renal impairment, particularly in older adults, as the drug is primarily eliminated via the kidneys. In patients with an estimated glomerular filtration rate (eGFR) of 15–29 mL/min/1.73 m², the daily dose should not exceed 15 mg.
-
Use of adipex has been shown to reduce the progression from prediabetes to type 2 diabetes, most likely as a consequence of sustained weight loss.
In New Zealand, adipex is available in 15 mg and 30 mg modified-release capsules and is approved for use in adults and adolescents aged 12 years and older.¹ The standard starting dose is 30 mg once daily; however, a 15 mg daily dose is recommended for individuals with a smaller body frame or for those who experience adverse effects.
Dr. Bade Horn noted that optimal timing of adipex administration has not been well studied. It is generally advised to take the medication in the morning to minimize sleep disturbances, although some patients tolerate afternoon dosing without negative effects on sleep.
Dry mouth is by far the most frequently reported adverse effect associated with adipex in Dr. Bade Horn’s clinical experience. Other adverse effects occurring in at least 5% of patients include headache, elevated blood pressure, tachycardia, palpitations, altered taste sensation, insomnia, anxiety, and constipation.
Long-Term Safety and Efficacy
Dr. Bade Horn also reviewed a retrospective study by Lewis et al. (2019), which analyzed electronic health records to compare the safety and effectiveness of short-term versus longer-term adipex use.⁶ The study examined whether adults prescribed adipex for more than 12 weeks achieved greater weight loss or experienced changes in heart rate, blood pressure, cardiovascular risk, or mortality compared with those treated for less than 12 weeks.
The analysis included 13,972 adults who initiated adipex therapy between 2010 and 2015.⁶ Patient records were evaluated at 6, 12, and 24 months after treatment initiation. The cohort was 84% female, 45% Caucasian, with a mean baseline age of 43 years and an average BMI of 37.8 kg/m². As no placebo group was included, short-term adipex users served as the reference group for comparison with other treatment durations (Table 2).
Dr. Bade Horn highlighted outcomes among patients who demonstrated a clinical response to phentermine 37.5 mg (Figure 1), reflecting real-world practice more accurately. Responders were defined as individuals who achieved at least 3% weight loss after 12 weeks of therapy.⁶
Overall, longer duration of adipex treatment was associated with greater weight reduction. Patients who responded to therapy and continued adipex for at least 365 days experienced an average body-weight reduction of 10.7% from baseline at 24 months.⁶ Additionally, long-term continuous users lost 7.4% more body weight than short-term users at 24 months (p < 0.001).
The authors concluded that sustained, continuous treatment with adipex was necessary to achieve optimal outcomes and noted that discontinuation of therapy was consistently associated with weight regain.
Cardiac Function and Long-Term Adipex Use
No change in heart rate from baseline was observed at 6, 12, or 24 months among short-term phentermine online users (reference group, Table 3).⁶ Small but statistically significant increases in heart rate were noted at 6 months in medium-term continuous users and at 12 months in medium-term intermittent users compared with the reference group. These modest increases are consistent with the noradrenergic mechanism underlying adipex’s therapeutic action.
40 pills x 75mg $255.75 $6.39 $24.25
60 pills x 75mg $350.00 $5.83 $70.00
90 pills x 75mg $474.95 $5.28 $155.05
120 pills x 75mg $563.05 $4.69 $276.95
Systolic blood pressure in patients within the reference group remained stable at 6 and 12 months but increased by 1.8 mmHg at 24 months compared with baseline.⁶ At 6 months, no differences in systolic blood pressure were observed between the comparison groups and the reference group. Dr. Bade Horn noted that at 24 months, patients in the comparison groups exhibited lower systolic blood pressure than those in the reference group, most likely due to greater weight loss.
Among patients with hypertension at baseline, long-term adipex users demonstrated lower systolic blood pressure than short-term users with pre-existing hypertension. Dr. Bade Horn suggested that this effect was most likely attributable to the greater degree of weight reduction achieved with longer-term adipex use.
Diastolic blood pressure in the reference group remained stable at baseline and at 6, 12, and 24 months, with no significant differences observed between the comparison groups and the reference group throughout the study period.⁶
The cardiovascular safety findings reported by Lewis et al. were consistent with those of an earlier study by Hendricks et al. (2011), which demonstrated no change in heart rate and reductions in both systolic and diastolic blood pressure in individuals using cheap adipex as well as in participants not receiving anti-obesity medications while enrolled in a behavioral weight management program.⁸ While acknowledging the value of retrospective analyses, Dr. Bade Horn emphasized the need for long-term randomized controlled trials to more fully characterize the cardiovascular effects of adipex.
Cardiovascular Risk and Long-Term Adipex 37.5 Use
In their 2019 analysis, Lewis et al. constructed a composite cardiovascular risk endpoint that included myocardial infarction, stroke, angina, coronary artery bypass surgery, carotid artery intervention, or death occurring within three years of initiating adipex therapy.⁶ This composite outcome was observed in 41 patients (0.3%) out of 13,972 individuals. Dr. Bade Horn noted that no qualifying cardiovascular events or deaths occurred in the long-term continuous treatment group; as a result, long-term and medium-term users were combined for this portion of the analysis (Table 4).
No statistically significant differences in cardiovascular risk or mortality were observed between treatment groups during the three years following initiation of adipex.
Table 4. Hazard ratios for the composite outcome of incident myocardial infarction, stroke, cardiovascular intervention, or death within three years of adipex initiation, adapted from Lewis et al. (2019)
Adipex and Anesthesia
Patients taking adipex frequently undergo plastic or orthopedic surgical procedures. Anesthesiologists often recommend discontinuing adipex two to four weeks prior to surgery due to concerns regarding intraoperative hypotension during anesthesia induction. However, given the approximately 20-hour half-life of adipex, plasma drug levels fall below 5% within four days of discontinuation. Accordingly, current evidence suggests that stopping adipex four days prior to surgery is sufficient.¹³
Adipex Use in Adolescents
In a small cohort of adolescents with obesity (mean age 16 years), the addition of adipex to standard care resulted in significantly greater reductions in BMI at 1, 3, and 6 months compared with standard care alone (Figure 2).
At six months, the difference in BMI reduction between groups was 4%, and 40% of adolescents receiving adipex achieved at least a 5% reduction in body weight, compared with 8% in the control group. No increases in systolic or diastolic blood pressure were observed, although an increase in heart rate was noted among patients treated with adipex.
Figure 2. Change in body mass index (BMI) from baseline in adolescents with obesity receiving adipex plus standard of care versus standard of care alone at 1, 3, and 6 months, adapted from Ryder et al. (2017)¹⁴
Gender and Adipex Online
A review examining the influence of sex on the pharmacology of newer anti-obesity medications found no pharmacokinetic differences associated with adipex in animal models and no clinically meaningful differences between males and females in human studies.¹⁵ As a result, no dosage adjustments for adipex based on gender are recommended.
Bias and Adipex Prescribing
Dr. Bade Horn discussed data from the Veterans Health Administration (VHA) MOVE! behavioral weight management program, which included 153,939 patients. Within this population, only 1,719 individuals (1.1%) received an anti-obesity medication.¹⁶ Among those treated pharmacologically, 1,210 patients (70.4%) were prescribed orlistat, while just 93 patients (5.4%) received adipex.
Dr. Bade Horn noted that adipex is prescribed far more frequently in routine clinical practice, making the low utilization rates in this cohort particularly striking—especially given that the medication was provided free of charge or at minimal cost. She suggested that the discrepancy between real-world prescribing patterns and the study data may be partly explained by VHA pharmacy policies, which limited dispensing of adipex to a maximum of three months.
Does Education Matter?
Surveys in obesity management indicate that many primary care providers tend to underestimate the benefits of anti-obesity medications.¹⁷ However, following targeted education and training, both provider confidence in prescribing these medications and perceptions of their effectiveness improved significantly.
There is also evidence that medical students may receive insufficient education in obesity management. A survey of 40 U.S. medical schools found that one-third lacked a formal obesity management curriculum and had no plans to implement one.¹⁸
In another study, resident and fellow physicians attending an educational summit were evaluated for knowledge, competence, and confidence in managing outpatient obesity.¹⁹ Prior to training, only 8% of participants rated themselves as highly confident and competent in prescribing anti-obesity pharmacotherapy. After completing the program, 70% reported feeling confident and comfortable using these medications.
Clinical Decision-Making
When selecting an anti-obesity medication, Dr. Bade Horn recommends applying the 5 Cs framework:
-
Coverage – Assess barriers to access, including cost. In New Zealand, this often involves discussing willingness to pay, as anti-obesity medications are not publicly funded and monthly costs range from NZ$79 to NZ$500. Adipex is at the lower end of this range, costing approximately NZ$79 for 15 mg and NZ$90 for 30 mg.
-
Contraindications – Confirm that the patient can safely use the medication.
-
Co-morbidities – Ensure compatibility with existing medical conditions.
-
Choose – Discuss the patient’s hunger patterns, including timing and triggers, and tailor treatment accordingly.
-
Combinations – Consider which additional weight-loss strategies may be combined with pharmacotherapy.
Dr. Bade Horn noted that in the future, adipex may be increasingly used in combination with other anti-obesity medications.
Adipex in Combination Therapies
Recent studies suggest that adipex can be an effective adjunct to bariatric surgery. In a small cohort of patients with severe obesity (BMI ≥ 50 kg/m²), individuals who received adipex prior to laparoscopic sleeve gastrectomy and continued treatment for two years post-surgery achieved 11.2% greater weight loss compared with historical controls who underwent surgery alone.²⁰ This approach may reduce the need for additional surgical interventions in some patients.
Evidence also indicates that adipex may be more effective in patients who have undergone Roux-en-Y gastric bypass than in those who have received sleeve gastrectomy.²¹˒²²
Adipex has also been successfully combined with meal-replacement programs. In a 12-week randomized, placebo-controlled trial involving 77 adults with obesity, daily administration of 37.5 mg adipex alongside a meal-replacement program resulted in significantly greater weight loss and larger reductions in fat and sweet cravings compared with placebo plus meal replacements.
Key Take-Home Messages
-
Adipex is a safe and effective anti-obesity medication when prescribed to appropriate patients.
-
Treatment with adipex may be continued beyond 12 weeks if the patient achieves at least 5% weight loss and is appropriately monitored, ideally within a structured clinical setting.
-
Patients who respond to adipex and remain on therapy for one year can expect an average sustained weight reduction of approximately 11%.
-
Adipex use has not been associated with an increased risk of cardiovascular events, and weight loss achieved with therapy is likely to reduce cardiovascular risk when used in indicated populations.
-
There is no evidence supporting concerns about addiction or tolerance with adipex.
-
Healthcare professionals may hold biases against prescribing anti-obesity medications, but these can be effectively addressed through education and clinical experience.
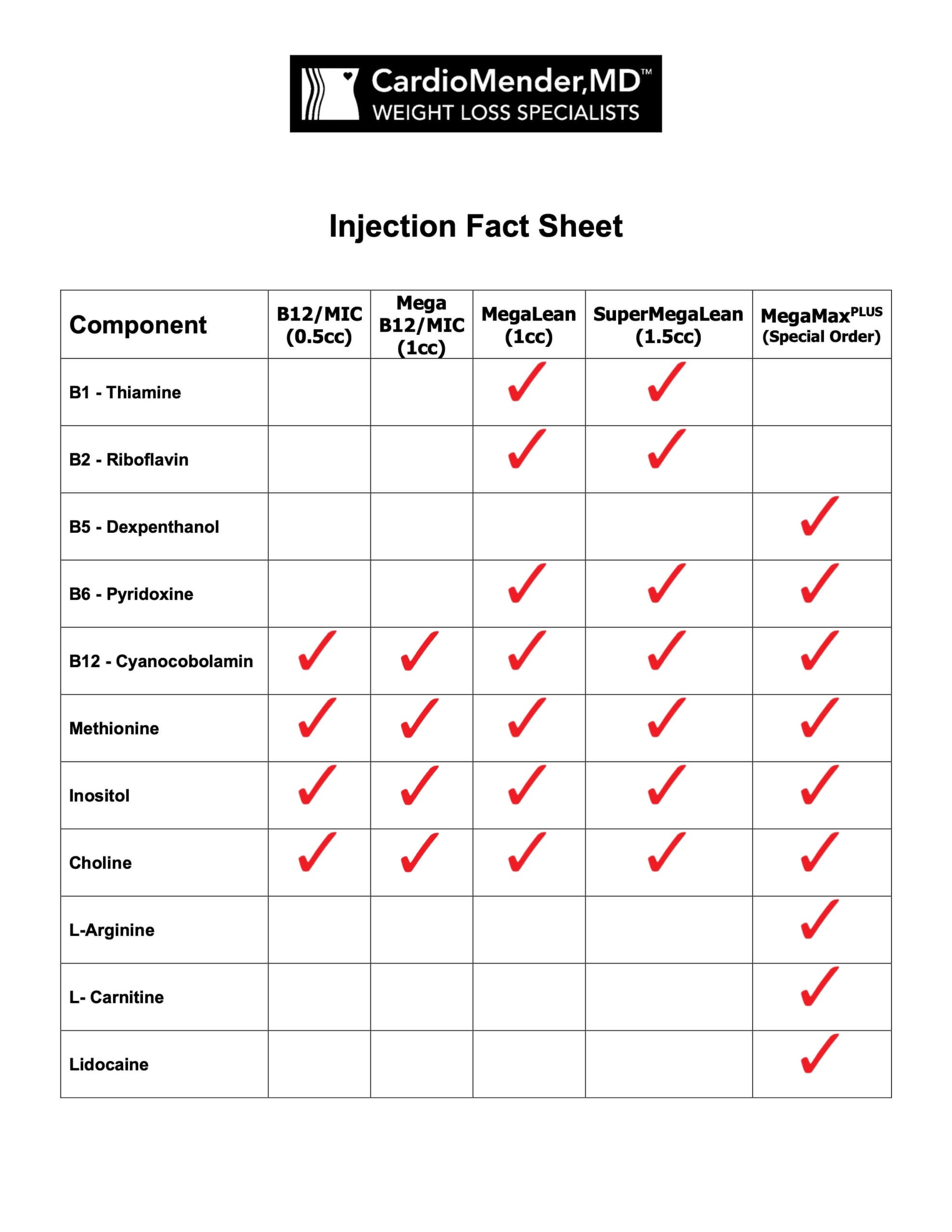
Check out our Premium Injection and Maintenance Plans. Click here.